Introduction
When I was diagnosed with type 1 diabetes, I was told that I will be able to live a normal life. What does a normal life mean, though? I have always been a fan of trekking, camping, and traveling. Also, I had just gotten into ultracycling. I did my first event, Istraland 2023, about 5 months before my diagnosis. Is ultracycling a part of a “normal” life? Many will answer this question with a resounding ’no’, but for some it is part of their lifestyle. I was afraid I would have to give up the more adventurous side of me.
Just a week after diagnosis I started experimenting with cycling as a type 1 diabetic. I had taken the advice from my doctors and lowered my insulin significantly hours before the start. I felt like I was prepared and was doing everything correctly. However, only 30 minutes into the ride, my blood sugar was plummeting already! I took a break, ate some food, and waited to continue my ride until I was sure my blood sugar was in range again. After twenty minutes, I realized that my blood sugar was now quickly rising, so I continued the ride. Another 30 minutes later, my blood sugar was again rapidly dropping! I had to stop again, eat food again, and wait again.. This is known as the blood sugar rollercoaster among type 1 diabetics and is one of the most frustrating things about being a diabetic. I was sweating profusely and I felt like throwing up from the amount of food I had consumed. One thing was clear.. participating in another ultracycling event was not possible until I figured this thing out.
I decided that I would be returning for the Istraland 2024 ultracycling event. Because I already completed this event the year before (as a non-diabetic), it would allow me to focus on diabetes management without worrying too much about all the other challenges that come with ultracycling. The general advice from the doctor was simply to eat food when I would go low. This sounds very simple, but I often experience stomach upset when I am doing long bouts of exercise and eat a ton of food at the same time. Also, this approach inadvertedly leads to the blood sugar rollercoaster as mentioned above. Therefore, the goal of this article is to show you how I manage to keep my blood sugar in range without consuming excessive amount of carbs during an ultracycling event. I will explain muscle physiology during exercise, hormonal responses to hypoglycemia, and how an understanding of these two can lead to good blood glucose control.
Muscle physiology and how to influence it
The first thing we need to understand is how muscles get their energy. There are two forms of energy, glucose (from carbohydrates) and ketones (from fat), and their relative contribution depends on many factors. Muscles have a local “glucose storage” in the form of glycogen. This allows the muscles to be active for a limited amount of time. During prolonged exercise glycogen stores run out and additional glucose needs to be delivered through the blood stream from the liver. Although muscles need insulin to take up glucose at rest, they can take up glucose without any insulin during contraction. Since insulin levels are low during exercise, most non-muscle cells will not be taking much glucose from the blood stream. This means that the energy delivery through glucose is concentrated on the active skeletal muscles.
The insulin-independent uptake of glucose by skeletal muscles also means that exercise can lead to hypoglycemia without any insulin on board. For this reason, both healthy individuals and type 1 diabetics need to take in sufficient carbohydrates to match the needs of their muscles. This is the common strategy in cycling and is commonly considered the best nutrition strategy to optimize performance. I used this method and it meant that I had to take in around 70g of carbohydrates per hour to avoid hypoglycemia. This is a lot of food and my stomach struggles to process that amount. Besides that, consuming such high amounts of carbohydrates can cause huge blood sugar swings in type 1 diabetics. This can partially be solved by micromanaging food intake, i.e. take 5g of carbs every 5 minutes. This sounds easy, but is challenging in practice and disrupts the “meditative” state of long cycling tours that I like so much.
This raises the question whether we can change our perspective. Instead of matching food intake to glucose uptake by the muscles, can we somehow match glucose uptake by the muscles to food intake? In other words, can we reduce the glucose utilization of skeletal muscles for a given exertion? It turns out that switching to a low-carbohydrate, high-fat (LCHF) diet in our daily lives makes this possible. If we cut out carbs from our diet, our body will start adapting its physiology to be more reliant on fat rather than glucose for energy. This process is often called ‘fat adaptation’. Note that the exact time required for fat-adaptation is not well-known, but it took me around 6 months to see the full range of effects. Many studies consider an adaptation period of less than 4 weeks, so it is unclear if the participants of these studies are truly fat adapted. Nevertheless, there are some insightfull studies out there. Let us have a look at two of them.
Carbohydrate and fat oxidation at endurance pace
The first study is by J.S. Volek et al1. In a 2-day study, they compared 20 ultra-endurance athletes of similar fitness levels. Half of them were on a HCLF diet and half were on a LCHF diet for at least 6 months. Peak fat oxidation and VO2max were measured on the first day. On the second day, they let the participants rest for 90 minutes after which they performed a running effort at 65% of VO2 max for 180 minutes. A VO2max of around 65% corresponds to a zone 2 bike ride, that is, a bike ride at endurance pace. Both glucose- and fat-utilization were measured before, during, and after exercise. We can see the results in the following figure.
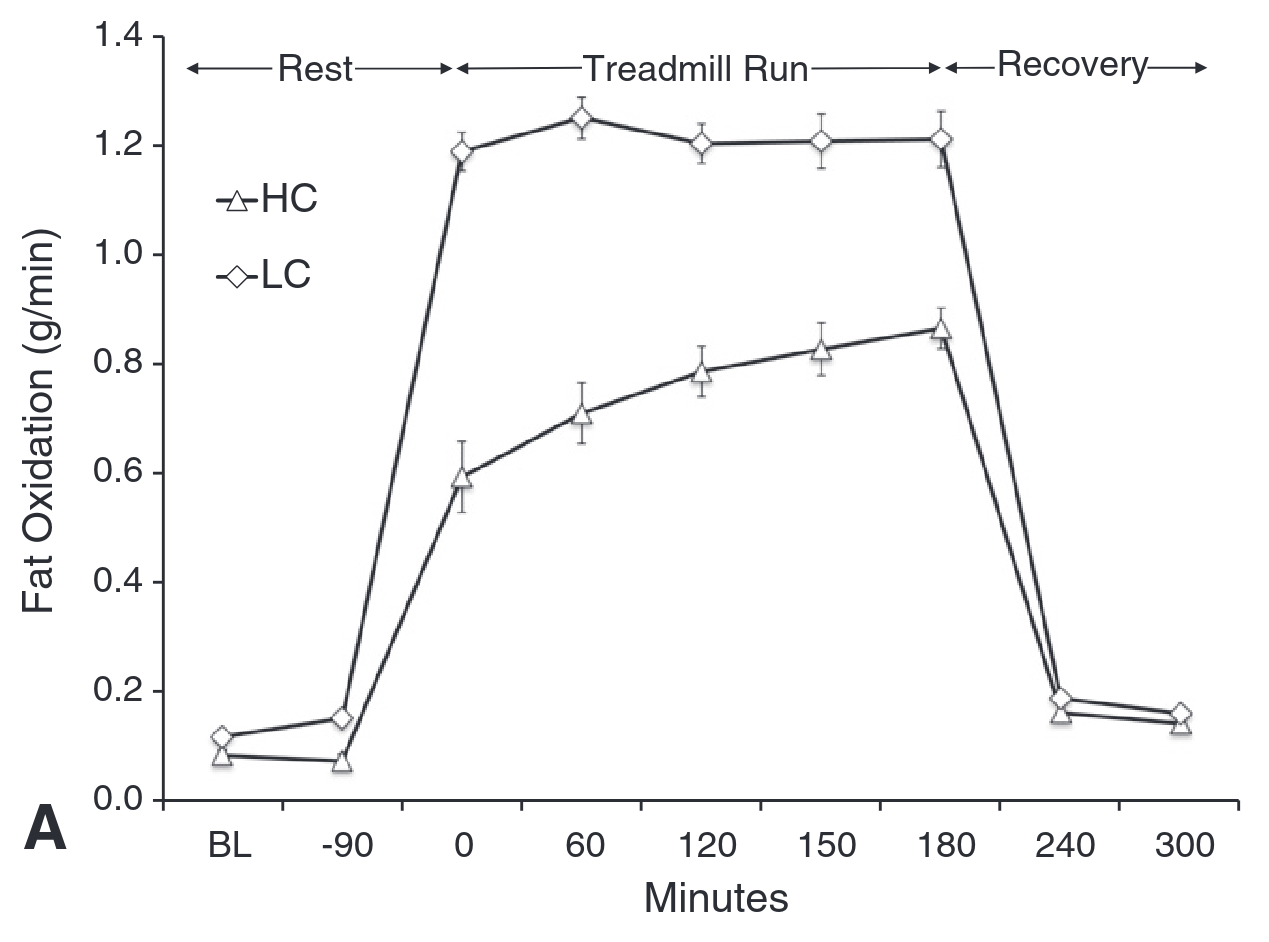
In the figure about carbohydrate oxidation, we can see that the carbohydrate oxydation in the LCHF group was less than 20% of that in the HCLF group! Remember from the introduction that I needed around 70 grams of carbohydrates per hour to avoid low blood sugar during cycling at endurance pace. This study considered runners instead of cyclists, but the physiology should be similar. Does this mean that I can lower this to less than 15 grams per hour by switching to a LCHF diet? We will find the answer to that further down in this article.
Energy derived from glucose at different exercise intensities
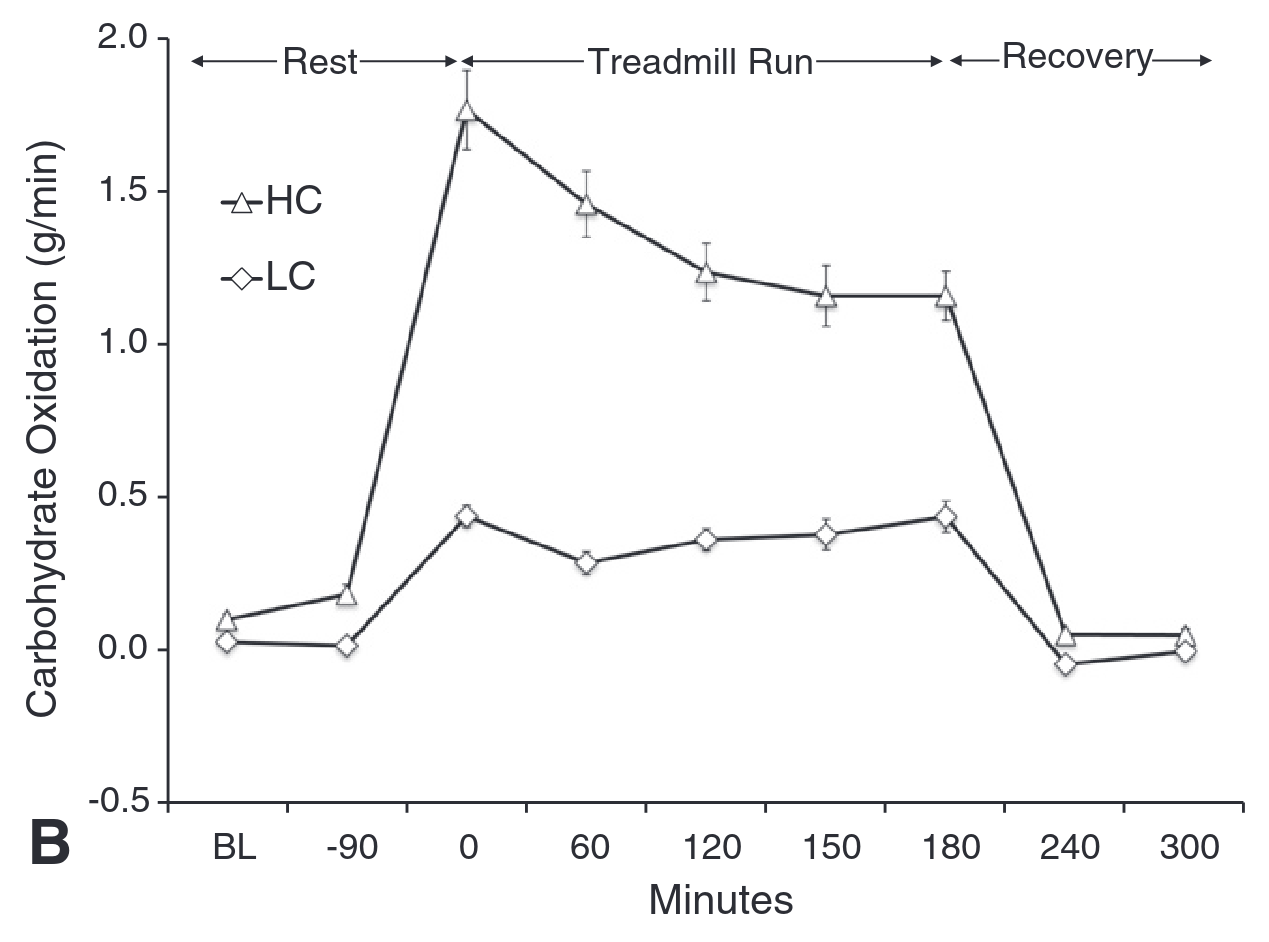
Let us now consider the question of what happens at different exercise intensities. It is well-known that carb consumption goes up and becomes the dominent energy source at high intensities. However, this notion is based on athletes following a HCLF diet. The question is whether this this still holds true for athletes on a LCHF diet. P.J. Prins et al2 considered exactly this question. They considered 7 athletes whose habitual diet was HCLF. They instructed them to follow a LCHF diet for a period of 42 days and confirmed proper execution of the diet through ketone measurements. Before and at the end of the dietary intervention, they measured energy contributions from fat and carbohydrates at different exercise intensities and summarized them in the following figure.
We observe again that carbohydrate oxidation at low intensities is MUCH lower after adopting to a LCHF diet. We also see that carbohydrate oxidation goes up significantly for exercise intensities close to VO2max. You might think that this means that exercising at such high intensities increases the risk for hypoglycemia. The opposite is true, because at such intensities the body releases adrenaline. Adrenaline promotes the release and production of glucose and thus often leads to hyperglycemia in type 1 diabetics as we will see later in the subsection on training.
Hormones and blood sugar
Although not optimal for performance, healthy athletes can keep doing exercise for significant amounts of time in a fasted state. Why is it that diabetics can not do this if they reduce their insulin intake sufficiently? In healthy individuals it is well-known that blood sugar is regulated through hormones. The most important of these hormones are insulin, glucagon, and adrenaline (or epinephrine). We will discuss how each of these hormones is involved in blood sugar regulation in a healthy individual and how this is different in a type 1 diabetic.
Insulin
All diabetics are aware of the role of insulin. Insulin signals to the cells that they can take up sugar from the blood stream for storage or recovery. In a health individual, the beta cells in the pancreas release insulin based on current blood sugar levels. When blood sugar is low or during exercise, very little insulin is released as a measure to avoid hypoglycemia. Indigineous insulin remains in the body for approximately 20 minutes. As a type 1 diabetic my immune system has attacked my beta cells and, therefore, they do not produce any insulin anymore. Instead, I inject insulin myself and, thereby, take over the role of the beta cells. Unfortunately, the insulin I have at my disposal (Lantus and NovoRapid) are very rough tools to work with. My meal-time insulin remains in the body for 3 to 5 hours and does not downregulate when exercising! We will see in the next chapter that muscles are able to take up glucose without any insulin during exercise. This means that exercise in combination with insulin can lead to rapid blood sugar drops up to five hours after injection. Fortunately, this is something we can easily control. Whenever we plan to exercise a lot, we make sure not to have excessive amounts of insulin on board (but we always keep some!). For that reason, we will assume throughout this article that we are only using basal insulin (Lantus in my case) and very low doses of that. This mimicks the low levels of insulin during exercise in a healthy body.
Glucagon
Whereas insulin promotes the absorption of sugar by cells, glucagon promotes the production or release of sugar. So, while insulin brings blood sugar down, glucagon brings it up. When blood glucose is below 3.9 mmol/L, glucagon is secreted by the alpha cells in the pancreas of healthy individuals. Unfortunately, it seems that the alpha cells are linked to the beta cells. The result is that alpha cells do not function in people with type 1 diabetes.
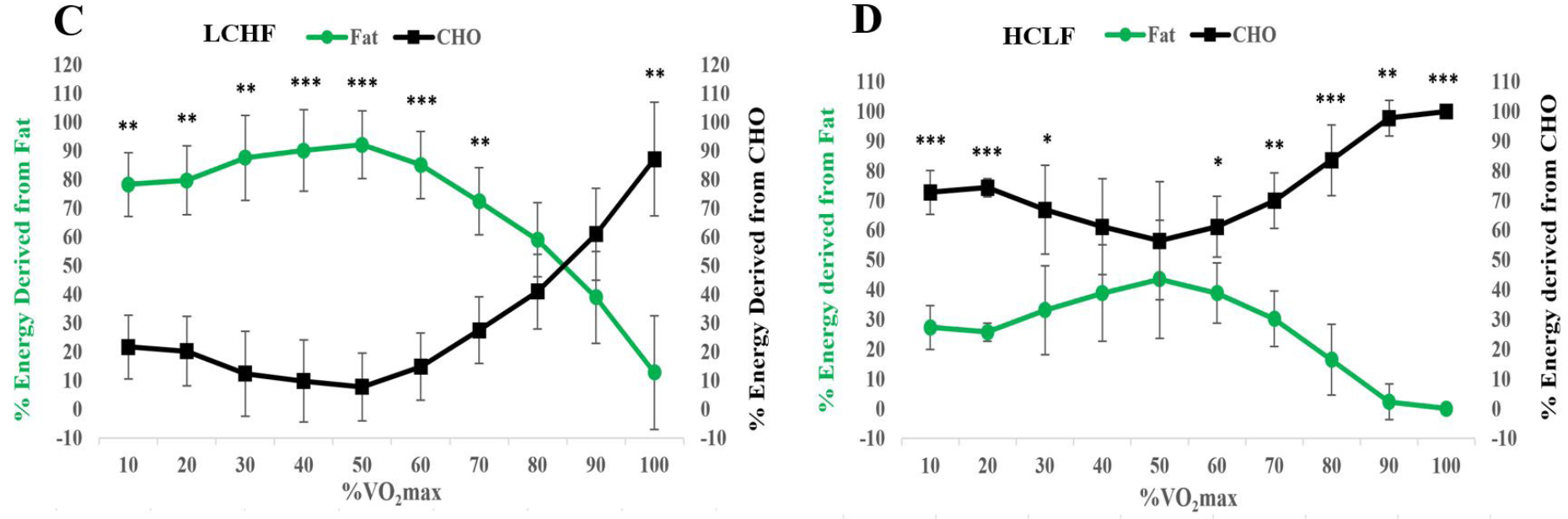
Let us have a look at a study by Bengsten et al3. They considered the glucagon response to hypoglycemia in patients with type 1 diabetes compared to healthy individuals. In total, nine type 1 diabetics and nine healthy individuals took part in the study. Both groups received insulin and sugar through continuous intravenous infusion to keep their blood glucose at fixed levels. In the group with type 1 diabetics, blood sugar was initially kept between 6 and 9 mmol/L. In the healthy group, initial blood sugar was left constant as controlled by the body itself. Then, insulin was administered to both groups such that they reached a hypoglycemic state with blood glucose levels below 2.9 mmol/L. Glucagon levels were measured at various instances during this process. You can find measured glucose and glucagon as a function of time in the following figures.
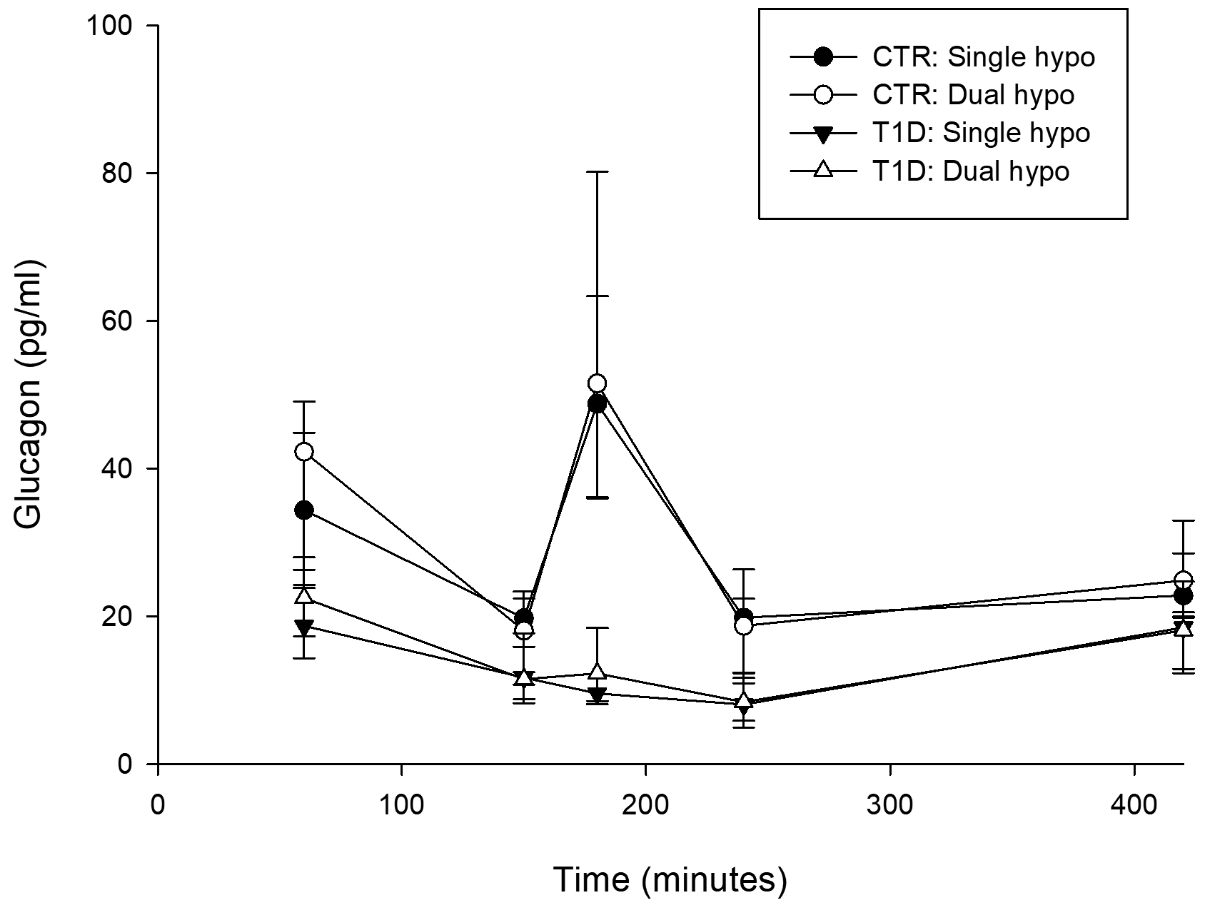
Note that the glucagon response in people with type 1 diabetes is basically absent! Unlike insulin, it is not common for diabetics to administer glucagon except in cases of emergency. However, simply eating glucose tablets mimicks the effect of glucagon and brings our blood sugar up rather quickly. We could argue that taking glucose tablets is some form of manual glucagon “replacement” by lack of a better word.
Adrenaline and other hormones
Other hormones that have an effect on blood sugar are adrenaline, norepinephrine, growth hormone, and cortisol. These hormones promote sugar production and release in a similar way as glucagon. Besides carbohydrate intake, type 1 diabetics rely exclusively on these hormones to avoid hypoglycemia! Unfortunately, there are some disadvantages to these hormones compared to glucagon. These hormones are less effective than glucagon and get activated at lower blood glucose levels. Also, it turns out that recent occurance of hypoglycemia prevents the release of these hormones in response to future hypoglycemia. Even a single event of low blood sugar leads to the reduced release of the above-mentioned hormones.
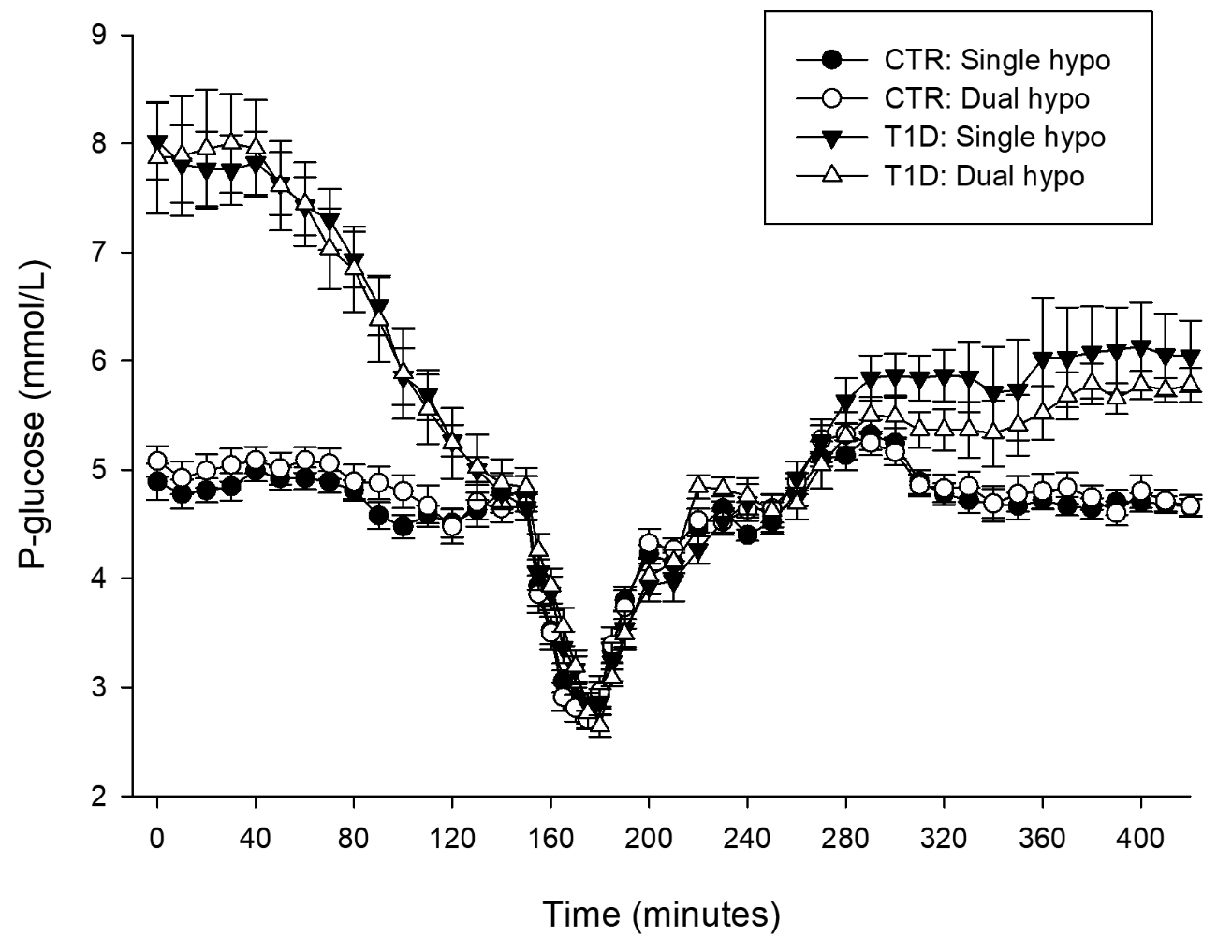
Dagogo-Jack et al4 considered two situations. Using a clamp technique they control blood sugar in participants to be either high or low in the afternoon. The next morning they used a the same methods to bring blood sugar to a low value. They measured the release of various hormones and compared them to each other. The most important results are given in the figure.
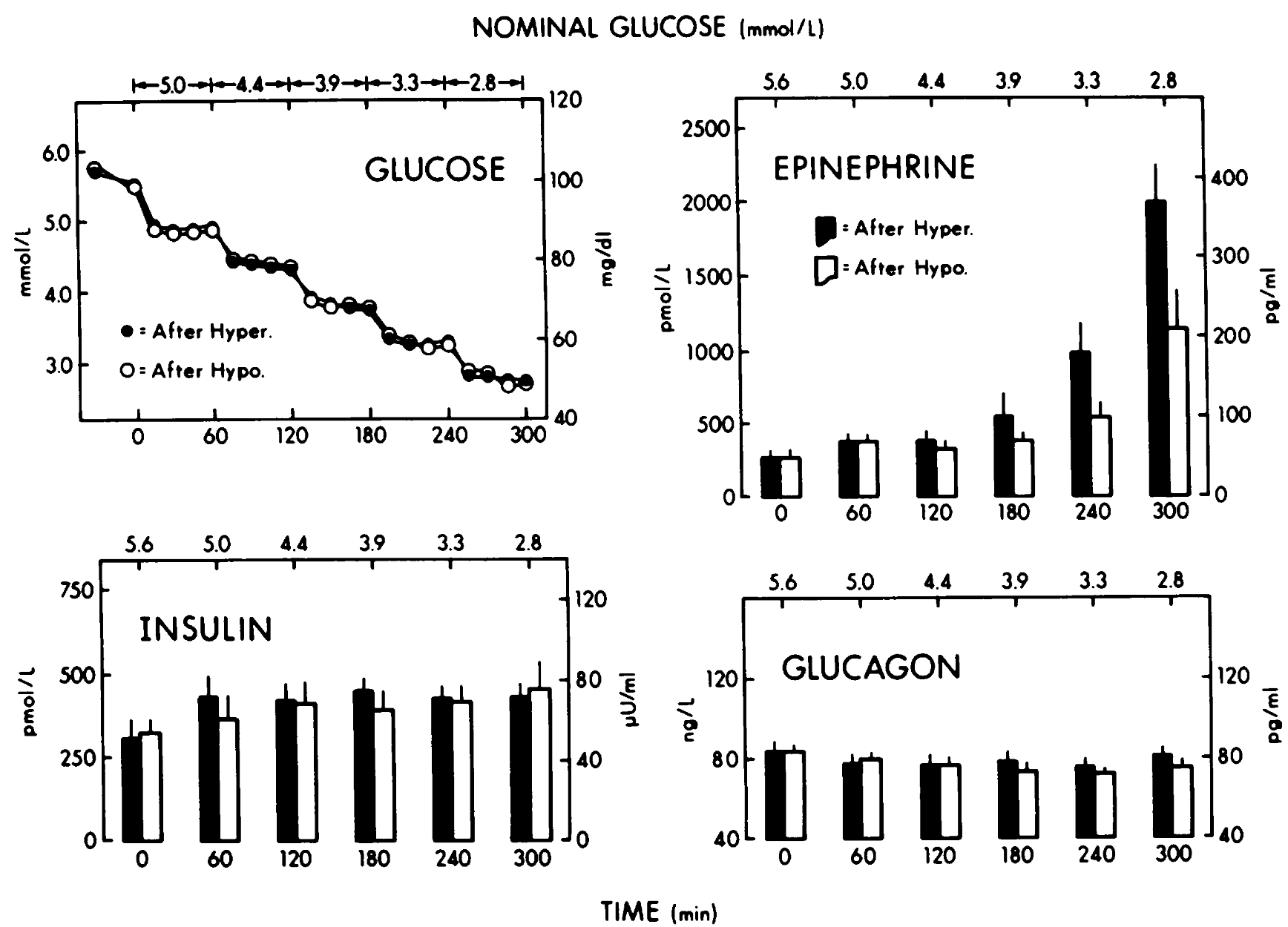
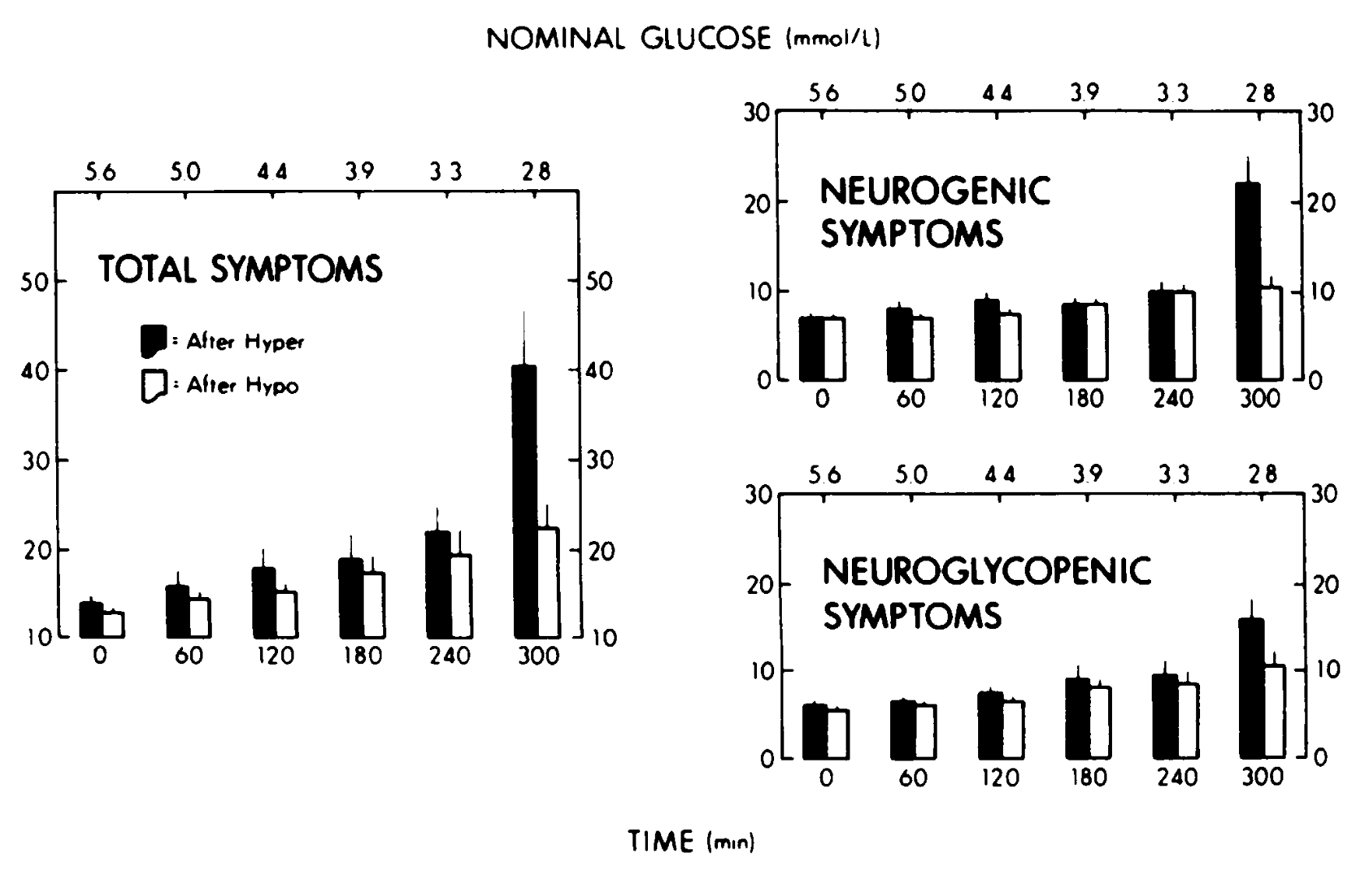
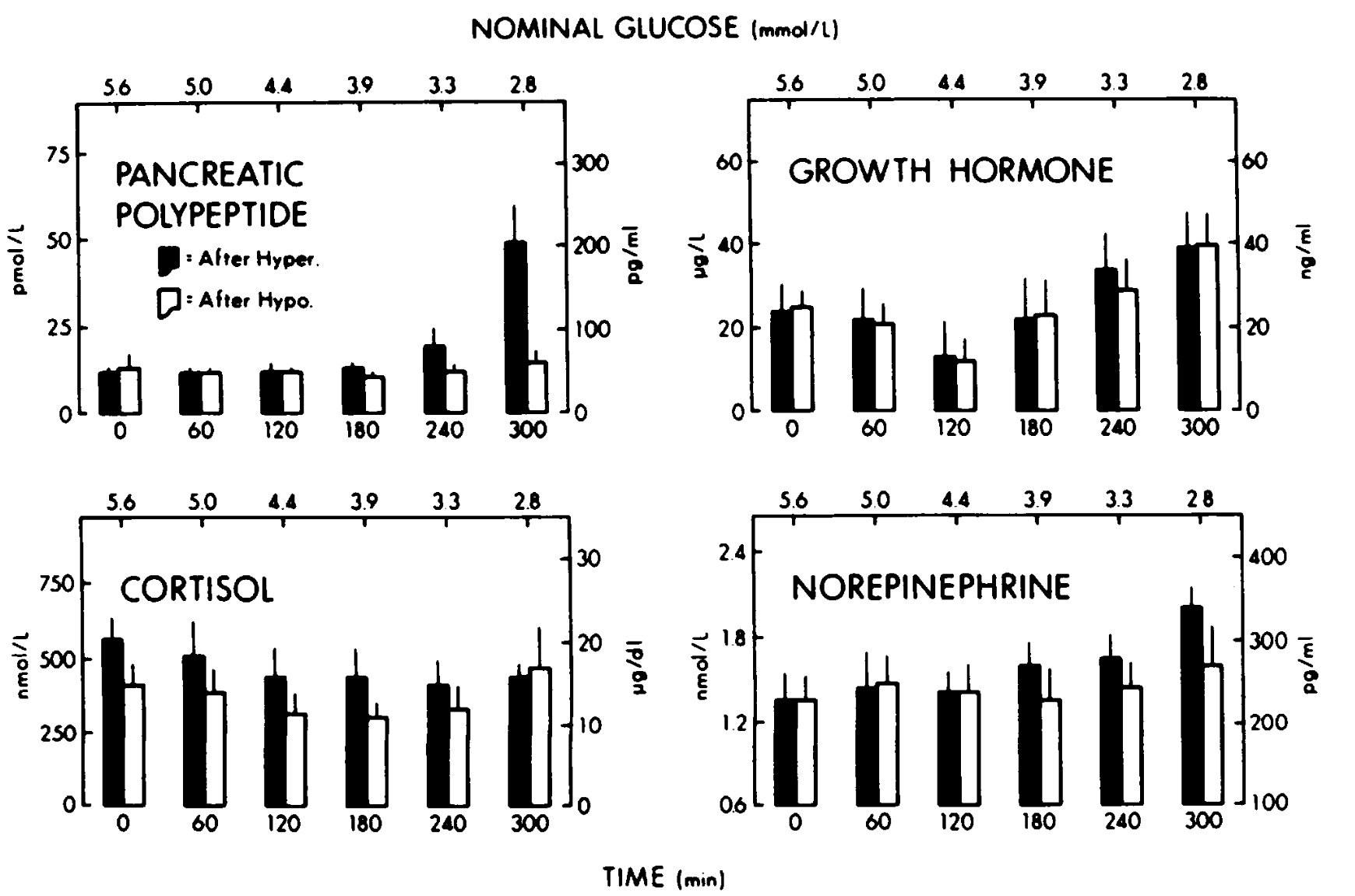
On one hand, it is good news that type 1 diabetics do still have some counterregulatory hormones in the absence of glucagon. On the other hand, we can clearly see from the graphs that the ability of a type 1 diabetic to release these counterregulatory hormones is significantly reduced after a hypoglycemic episode. This can lead to a vicious cycle, where the frequency of hypoglycemic episodes increases dramatically! If you have frequent low blood sugar, your body will eventually completely lose its ability to counteract them. This is extremely dangerous! Therefor, it should be of highest priority to avoid low blood sugar (<3.9mmol/L)! The good news is that the response can also be restored in a relatively short amount of time of around two weeks without low blood sugar5. Therefore, in the case of low blood sugar, I make my target blood sugar slightly higher for the following two weeks to avoid the vicious cycle.
My insulin and nutrition strategy
The above sections give us a good understanding of the different physiological aspects that can have an effect on our blood sugar during exercise. Since the reduced reliance on carbohydrates has greatly impacted my enjoyment of cycling, I choose to follow a LCHF diet in my daily life. This includes both heavy training weeks as well as rest weeks, but I do always correct for blood sugar if it is close to 3.9 mmol/L with glucose tablets or whatever seems appropriate. I have different strategies for training and races. However, in both cases, I make sure I have sufficiently low amounts of insulin on board. I might write a future article about my exact insulin strategy, but the basic idea is that we keep insulin low during exercise.
Training
My structured training consists of three types of training, i.e. threshold, HIIT, and zone 2 training. During the week I train mostly in the morning before I go to work and in winter this is mostly on my indoor bike. I collected data for the workouts that last around 2 hours and were performed fasted (without any blood glucose tablets for corrections). Note that, although fasted training is interesting, 2 hours is not enough to deplete glycogen storage in the muscle. It does give us a large enough set of data to get an idea of the average blood glucose response to these workouts. Due to different types of blood glucose responses, I will split the workouts in two groups: aerobic (zone 2 workouts) and anaerobic (threshold or HIIT). To give you an idea of what my heartrate looks like during a training I took two sample workouts from both groups and plotted my heartrate below. My threshold heartrate is around 182 beats per minute and my max heartrate is just above 200. I also plot the blood glucose response to both types of exercise.
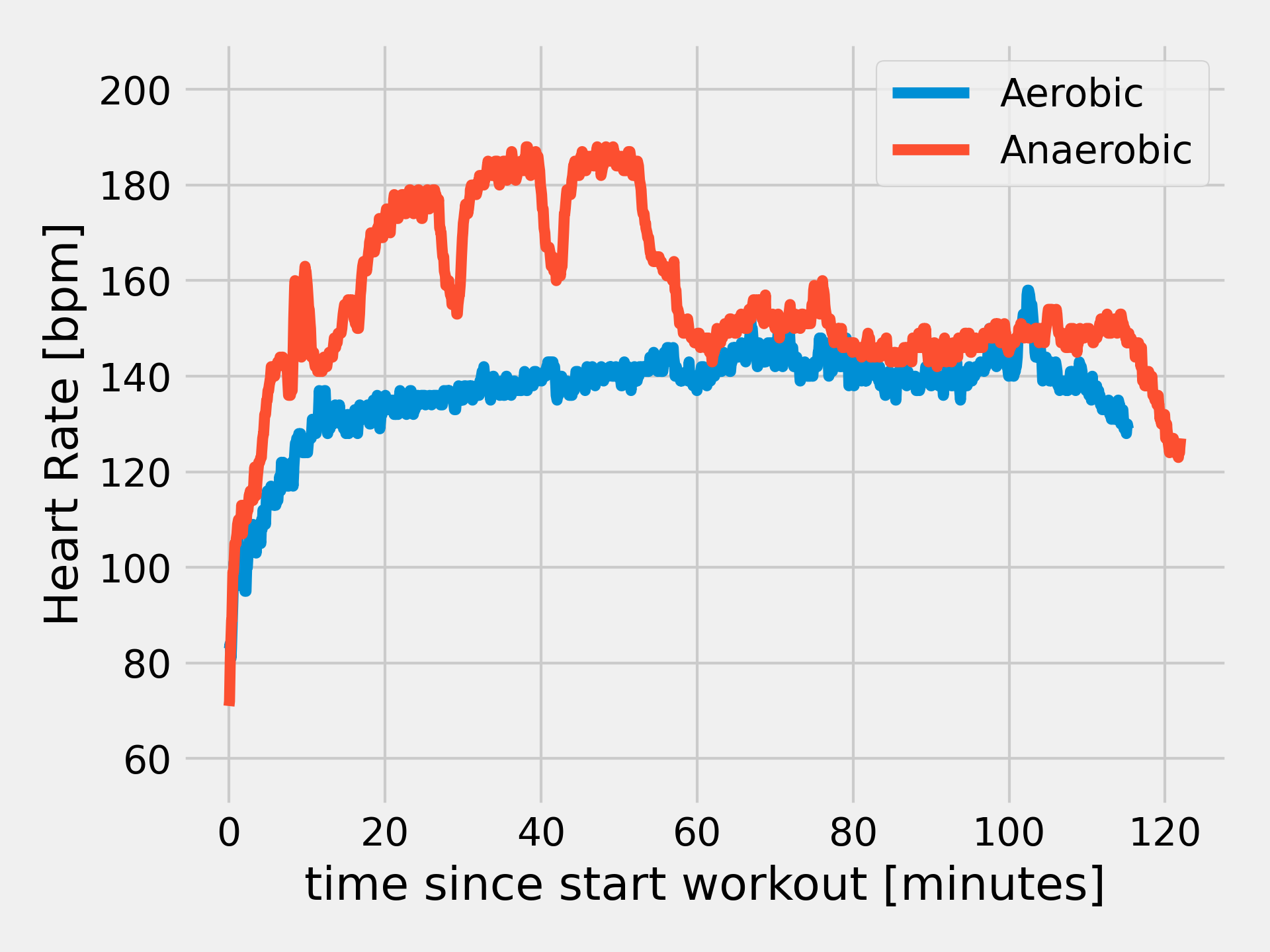
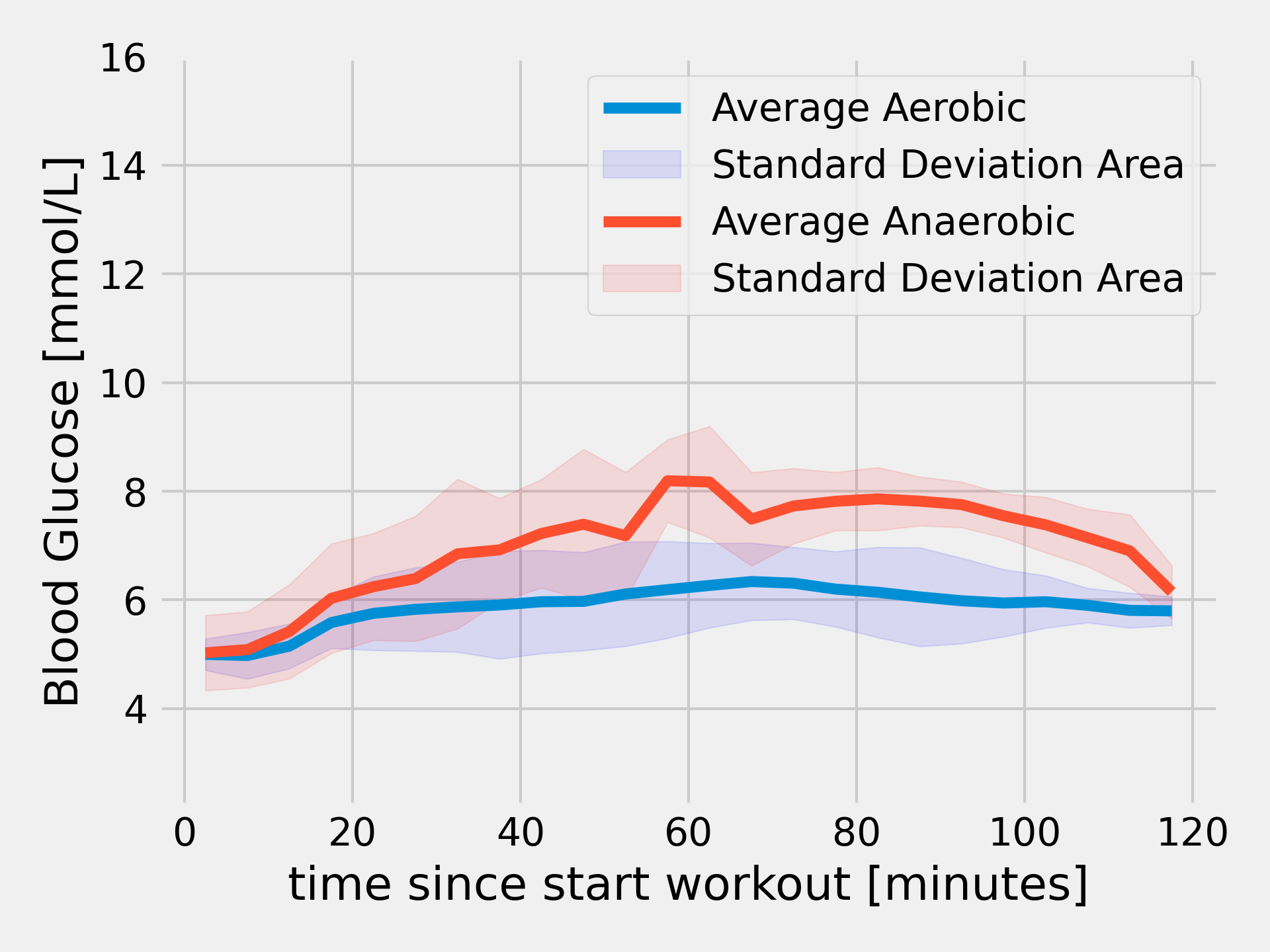
I observe no hypoglycemic events anymore during these workouts! That is a great feeling and really gives me some of my confidence back. The aerobic workouts show an average blood glucose that reaches around 6 mmol/L. This is not within the range of a fasted, healthy human being (3.9 - 5.7 mmol/L), but very close! Also, I noticed that during exercise my CGM consistently reports around 1 mmol/L too high. This is probably due to heat, which can affect accuracy of blood glucose sensors6. During anaerobic exercise, my blood sugar reaches much higher around 8 mmol/L due to adrenaline release as described before. Although not ideal, it is much better than going low. My ketones are often around 1.5mmol/L and I have never seen them above 3.0 mmol/L. This indicates nutritional ketosis, not diabetic ketoacidosis7.
Istraland 2024 ultracycling event
My blood glucose response to workouts gives a part of the picture. However, it does not give us any information of how blood glucose behaves in the “real world” or when glycogen stores deplete. Therefore, I will share my food strategy with you for the Istraland 2024 ultracycling event. This event is a mix of gravel, singletrack, and some tarmac. I recorded my ride using my Garmin and I finished in 33 hours and 41 minutes of which I had a moving time (time pedaling) of 31 hours and 5 minutes. Here is my recorded track:
My food strategy was simple. Whenever my blood glucose threatened to go low or whenever I felt like eating, I would eat. This could be either low-carb or high-carb foods. In the end, I ate the following foods:
| Food | Quantity | Net Carbs | Fat | Protein | Calories |
|---|---|---|---|---|---|
| Salted Macademia Nuts | 100g | 5.6g | 76g | 9.3g | 756kcal |
| BeKind Bar | 3 x small | 27g | 44.4g | 16.8g | 591kcal |
| Full Fat Greek Yoghurt | 100g | 3.5g | 10g | 4.4g | 122kcal |
| Prosciutto Meat | 200g | 1g | 34g | 60g | 604kcal |
| Smoked Chicken Breast | 100g | 1.9g | 1.2g | 20g | 99kcal |
| Agave Syrup | 150g | 112g | 0g | 0g | 450 kcal |
| Glucose Tablets | 8 x 3g | 24g | 0g | 0g | 96kcal |
| Total | 175g | 165.6g | 110.5g | 2'718kcal |
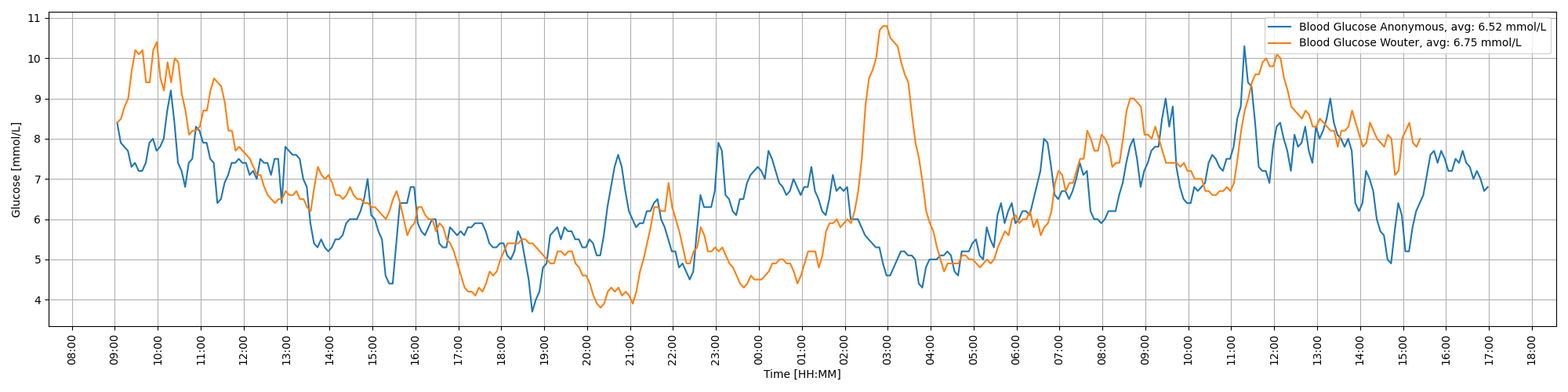
Note that my Garmin estimates that I burned a total 13'124 calories (resting + active). This means that I was in a deficit of about 10'000 calories! Although I felt strong throughout the race, I think optimal performance would require more calorie intake. I always struggle to keep eating food during such events. Eating around 300 calories per hour for 34 hours straight while exercising is not as easy as it seems! I only ate 175 grams of carbs or 5 grams of carbs per hour, which debunks the theory that we need carbs to complete endurance events. This agrees with the 10 grams of carbs per hour needed in healthy individuals on a LCHF diet8. Of course, one could argue that my performance would have been better with carbs, but I did not feel weak by any means. I did not have any serious hypoglycemic event, so it seems that the above theory really translates to reality. I compared my blood sugars to a carbohydrate-fueled rider taking part in the same event. Our blood sugars are very similar and the averages almost match. If non-diabetics cannot even achieve blood sugars within the range of 3.9 to 5.7, why would we expect a diabetic to? For that reason, my requirements for blood sugar are a bit looser during such events. The following picture shows the data.
Conclusion
In this article, I described how I made my blood sugar stable and predictable for prolonged exercise as a type 1 diabetic. In order to achieve that, we keep insulin levels low (both basal and bolus), consume a LCHF diet to reduce reliance on carbohydrates during exercise, and avoid hypoglycemia at all cost to keep our hormonal response to hypoglycemia. These three simple points allow me to do training up to 2/3 hours in a fasted state. Also, I completed the Istraland 2024 ultracycling event by consuming around 5 grams of carbs per hour and no hypoglycemia. Although I am not sure whether this leads to optimal performance, it definitely leads to optimal enjoyment for me. In the end, that is what counts for me.
I have chosen not to talk about the health benefits and drawbacks of a LCHF diet. Although it allows for great blood sugar control, there is an issue with increased LDL cholesterol in some people. For me personally, this was not a problem and my cholesterol is fine. Please, consult a doctor before starting such a diet.
J.S. Volek et al, “Metabolic characteristics of keto-adapted ultra-endurance runners” (https://www.metabolismjournal.com/article/S0026-0495(15)00334-0/fulltext) ↩︎ ↩︎ ↩︎
P.J. Prins et al, “High fat diet improves metabolic flexibility during progressive exercise to exhaustion (VO2max testing) and during 5 km running time trials” (https://www.termedia.pl/High-fat-diet-improves-metabolic-flexibility-during-progressive-exercise-to-exhaustion-VO-2-max-testing-and-during-5km-running-time-trials,78,47083,1,1.html) ↩︎ ↩︎
Bengtsen et al, “A Human Randomized Controlled Trial Comparing Metabolic Responses to Single and Repeated Hypoglycemia in Type 1 Diabetes” (https://doi.org/10.1210/clinem/dgaa645) ↩︎
S.E. Dagogo-Jack et al, “Hypoglycemia-associated autonomic failure in insulin-dependent diabetes mellitues. Recent antecedent hypoglycemia reduces autonomic responses to, symptoms of, and defense against subsequent hypoglycemia. (https://doi.org/10.1172/jci116302) ↩︎
K. Runyan, “Master Type 1 Diabetes” ↩︎
J.S. Volek and S.D. Phonney, “The Art and Science of Low-Carbohydrate Performance” ↩︎
P.J. Prins et al, “Carbohydrate ingestion eliminates hypoglycemia and improves endurance exercise performance in triathletes adapted to very low- and high-carbohydrate isocaloric diets” ↩︎